Abstract
Introduction: We have previously shown that older age and increased NLR were associated with worse outcomes among patients with hematologic neoplasms diagnosed with COVID-19 from March to June 2020. We sought to perform an updated and expanded analysis including follow-up data on the original patient cohort as well as evaluation of additional COVID cases among the hematologic neoplasms population up until February 2022.
Methods: A retrospective analysis of patients with hematologic neoplasms diagnosed with COVID-19 from March 17th, 2020 to February 1st, 2022 was conducted. Subjects included were censored at last point of contact. Variables collected included age, gender, race/ethnicity, hematologic diagnosis, cancer treatment status, date of COVID-19 infection, COVID-19 vaccination status, absolute neutrophil and lymphocyte counts, need for hospital and/or intensive care unit (ICU) admission, oxygen therapy, intubation, length of stay (LOS), and COVID-related and all-cause mortality. For survival analysis, associations between hematologic diagnosis, cancer treatment status, age, gender, race/ethnicity, neutrophil-to-lymphocyte ratio (NLR), date of COVID-19 infection, COVID-19 vaccination status, and overall survival (OS) were assessed using the Kaplan-Meier method with logrank test. A competing risks analysis was performed to assess COVID-related and all-cause mortality using Gray's test for comparing incidence curves. Univariate associations between NLR and hospital and/or ICU admission, oxygen therapy, and LOS were assessed using Fisher's and Kruskal-Wallis tests for categorical and continuous variables, respectively.
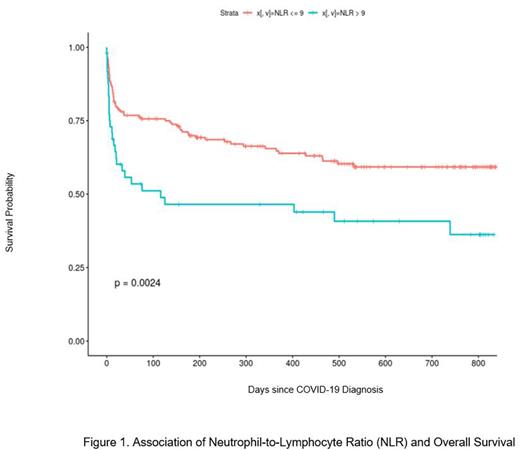
Results: A total of 248 subjects with hematologic neoplasms and COVID-19 infection treated in Montefiore Health system were identified. One-hundred and sixteen (47%) subjects were undergoing active treatment, including 84 (34%) receiving conventional chemotherapy agents, 19 (7%) targeted therapy, 3 (1%) immunotherapy alone, and 10 (4%) combination therapy. Of those subjects, 63 (55%) experienced delay or discontinuation of treatment due to COVID-19 infection. Thirty-two (13%) had received one or more COVID-19 vaccine doses at time of COVID-19 diagnosis. Sixty-two (25%) subjects expired as a result of COVID-19 disease at the time of analysis. Disease type, treatment status, race/ethnicity, age, gender, date of COVID-19 infection, and COVID-19 vaccination status showed no significant association with mortality. Age older than 70 and NLR >9 were significantly associated with worse OS (p=0.0012 and p=0.0024, respectively). Competing risk analysis further showed that age over 70 and NLR >9 were associated with COVID-related mortality, but not all-cause mortality (p=0.0002 and p=0.002717, respectively). NLR >9 was significantly associated with ICU admission (p=0.0322) and oxygen therapy (p=0.0155), but not hospital admission (p=0.0883), LOS (p=0.8819), or intubation though the latter trended toward significance (p=0.06778).
Conclusions: Despite the advent of the COVID-19 vaccine and new therapeutics, infection continues to portend adverse outcomes for many patients with hematologic neoplasms. Worse prognosis for patients over 70 years old persisted in our updated analysis. In addition, across multiple COVID-19 variants during the past two years, high NLR continues to correlate with illness severity including ICU admission and oxygen therapy, and COVID-related mortality among the hematologic neoplasms population. Elevated NLR may represent a useful prognostic to not only identify high-risk hematologic neoplasm patients, but also guide therapeutic interventions, and warrants further investigation.
Disclosures
Chaitowitz:Pharmacosmos: Other: Consulting. Shastri:Janssen: Consultancy; Rigel Pharmaceutical: Membership on an entity's Board of Directors or advisory committees; NACE: Honoraria; Kymera Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding. Verma:Throws Exception: Current equity holder in publicly-traded company; MedPacto: Research Funding; Incyte: Research Funding; BMS: Research Funding; Jannsen: Research Funding; Stelexis Therapeutics: Current equity holder in publicly-traded company; Stelexis Therapeutics: Consultancy; GlaxoSmithKline: Research Funding; Curis: Research Funding; Acceleron Pharma: Consultancy; Novartis: Consultancy, Research Funding; Eli Lilly and Company: Research Funding; Celgene: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal